-
Home
-
Patient Positioning in Bed: Benefits and Techniques
Patient Positioning in Bed: Benefits and Techniques
May 23, 2023
Bed positioning is a crucial aspect of patient care that, when done properly, can help improve comfort, alleviate pain, and promote safety. This resource is intended to provide insight into the benefits of and techniques for correct bed positioning in healthcare settings such as hospitals or long-term care facilities. We will also highlight additional support devices that may be used to enhance patient comfort and safety.
Importance of Proper Bed Positioning
While it might seem like a small aspect of patient care, proper bed positioning is incredibly important. Incorrect positioning can cause discomfort and pain, and may even result in a decline in health. When patients are not positioned correctly in their beds, they are at risk of experiencing pressure sores, muscle strain, difficulty breathing, and contractures.
Benefits of Bed Positioning
Correct bed positioning offers numerous benefits to medical patients, including:
- Relieving pressure on the body, which helps prevent bedsores, skin breakdown, and other pressure injuries
- Relieving pain and discomfort caused by various medical procedures or surgeries
- Improving breathing and circulation, allowing for better oxygenation of different body parts
- Helping prevent falls by keeping the patient within the confines of the bed
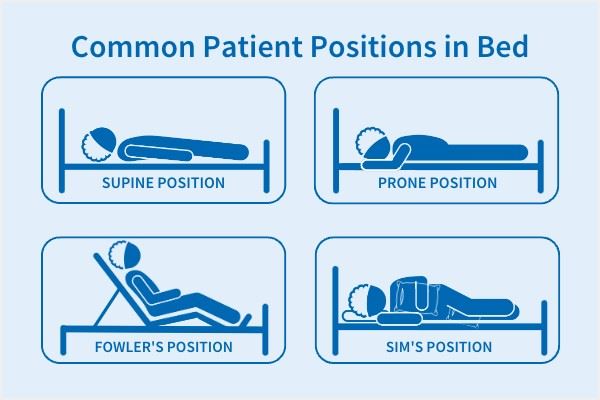
Common Patient Positions in Bed
There are a variety of positions in which the patient can be placed while in bed, each with its own advantages and risks. Below, we will outline some of the more common bed positions utilized and highlight the best use cases for each.
- Supine Position: The patient lies flat on their back, often with the head and shoulders slightly elevated.
- This position is ideal for post-surgical recovery and general examination but poses an increased risk of pressure ulcers and nerve damage. When positioning a patient in Supine, be sure to pad weight-bearing surfaces and bony prominences and monitor skin condition.
- Fowler’s Position: The head of the patient’s bed is elevated between 45 and 60 degrees.
- This promotes chest and lung expansion and is useful for patients with cardiac, respiratory, or neurological problems. However, it also increases the risk of neck contractures. Patients in this position should occasionally rest without a pillow to allow full neck extension.
- Orthopneic or Tripod Position: The patient is in a sitting position with an overbed table in front to lean on, generally padded with pillows.
- This promotes lung expansion and is great for patients with difficulty breathing, especially those who have trouble exhaling as they can press against the edge of the overbed table. Fall risk is increased, however, and caregivers should ensure that patients in this position are closely monitored and can safely sit back in bed.
- Prone Position: The patient lies face down with a pillow under the head and a roll or pillow under the abdomen and knees.
- This position allows full extension of the hip and knee joints and helps prevent flexion contractures. It also promotes drainage from the mouth and is useful for unconscious clients or those recovering from surgery on the mouth or throat. However, this position can put increased stress on the trunk and back, and it should not be used with patients who have spine problems.
- Lateral Position: The patient lies on one side with their top leg in front of the bottom leg and the hip and knee flexed.
- This position helps relieve pressure on the sacrum and heels and promotes proper back alignment. In this position, support pillows or positioners are needed to correctly and comfortably position the patient and ensure even weight distribution.
- Sims’ Position: The patient assumes a posture halfway between lateral and prone —the lower arm is positioned behind the body, the upper arm is flexed at the shoulder and elbow, and the upper leg is flexed at the hip and knee with a pillow or positioner between the legs.
- This position helps prevent aspiration of fluids and reduces pressure on the lower body. In this position, it is important to place pillows or positioners for support under the patient’s head and upper arm to prevent internal rotation.
- Trendelenburg Position: The head of the patient’s bed is lowered and the foot of the bed is raised.
- This position promotes venous return for hypotensive patients but presents an increased risk of dyspnea. Patients in this position should be moved slowly and gradually.
- Reverse Trendelenburg Position: The head of the patient’s bed is raised and the foot of the bed is lowered.
- This position is great for patients with gastrointestinal problems, as it helps minimize esophageal reflux, but poses an increased risk of rapid hypotension. As with Trendelenburg, patients in this position should be adjusted slowly and gradually.
Tips for Positioning a Patient in Bed:
The process of positioning a patient in bed should be smooth, safe, and comfortable for both the caregiver and the patient. Below are some general tips to help accomplish this goal.
- Start by explaining the positioning process to the patient.
- Encourage the patient to assist if they are able to—this will help the positioning process go more smoothly, promote patient independence, and reduce strain on the caregiver.
- Ensure that there is an adequate number of caregivers present to safely position or move the patient.
- Always ensure the position is comfortable for the patient, checking for any pressure on bony areas such as the hips and shoulders.
- Use proper body mechanics when positioning or moving a patient. Caregivers should keep the back, neck, and pelvis aligned, flex the knees, keep the feet wide apart, and use the arms and legs rather than the back.
- Reposition or turn the patient according to protocol every two hours or so to minimize discomfort and pressure injuries.
Turning Protocols
Turning protocols and pressure relief surfaces are also essential aspects of bed positioning. Turning schedules are developed to help prevent pressure ulcers and bed sores, which are caused by continuous pressure on a single body part. Changing the patient's position every few hours helps relieve this pressure and allows caregivers to check the patient for skin breakdown or sores.
Turning a patient generally requires at least two caregivers, and assistive devices should be used whenever possible. One such device, the AliMed® No-Lift TURNER™, is a flat tube of fabric with a slippery interior surface that is used as you would a draw sheet. Though placement generally requires two people, usually only one caregiver is needed to turn the patient once the TURNER is in position.
Additional Support Devices
Pressure relief surfaces and alternating pressure mattresses can be added to the bed to enhance patient comfort and safety. These devices help reduce the risk of pressure injuries and can also aid in the healing process of existing ones.
- Pressure-Relief Mattresses: The Med-Aire 8” Mattress utilizes both alternating pressure and low air loss to optimize pressure redistribution and manage skin maceration. It helps prevent, treat, and manage pressure injuries in both long-term care and acute-care settings.
- Side-Lying Wedge: The AliMed® Bed Positioning Wedge is used for side-lying support and trunk stabilization to maintain positioning schedules and help prevent pressure injuries.
- Heel Pillow: The AliMed® Foot Stabilizer is used to elevate the heel and relieve pressure, providing comfortable, breathable support with malleoli and heel protection. When used in a side-lying position, ankles are protected by side cutouts.
The patient's safety and comfort should always be a top priority. By following proper bed positioning techniques and utilizing support devices, medical professionals can help prevent additional pain, discomfort, and complications for patients in bed.
Explore our Surgical Patient Positioning Product Guide for additional information on products or devices for surgical patient positioning.