-
Home
-
Is the Chronic Problem of Miscommunication a Patient Safety Issue?
Is the Chronic Problem of Miscommunication a Patient Safety Issue?
August 6, 2019
Effective communication at healthcare facilities is critical to providing the very best care to patients. Yet, miscommunication remains a consistent problem. Miscommunication is not just inconvenient; it can be harmful patients. In studies of intensive care units at multiple sites, poor collaborative communication among nurses and physicians caused a 1.8-fold increase in patient risk-adjusted mortality and length of stay.1 A study by CRICO Strategies, a research and analysis offshoot of the company that insures Harvard-affiliated hospitals, found communication failures were linked to 1,744 patient deaths in five years and $1.7 billion in malpractice costs.2 Further, a study from the University of California, San Francisco, found more than a quarter of hospital readmissions could actually be avoided if there were simply better communication among healthcare teams and between providers and patients.3
Research from the Joint Commission found that communication failures were at the root of over 70% of sentinel events, defined as unexpected occurrences involving death or serious physical or psychological injury, or the risk thereof.4 When surveyed, nurses identified communication issues with physicians as one of the two most highly contributing factors to these types of events. Exacerbating the problem is the sheer number of hand-offs every day. In just one typical teaching hospital, there can be more than 4,000 provider-to-provider hand-offs each day.5
Inadequate hand-off communication
Effective communication and collaboration between healthcare providers is especially critical during a hand-off. A hand-off is a transfer of patient care responsibility, including passing patient-specific information from one caregiver to another or from one team of caregivers to another for the purpose of ensuring the continuity and safety of the patient’s care. The potential for patient harm is introduced when the receiver gets information that is incomplete, inaccurate, misinterpreted, or not timely.
Failed hand-off communication scenario
The following scenario illustrates a failed hand-off communication, where critical information was not effectively communicated to the receiver.6 A U.S. soldier sustained injuries after he walked over an explosive device in Afghanistan. During a trauma surgery, his right leg below the knee and right arm were amputated. He also suffered moderate brain injury and intermittent pain. Unaccompanied by caregivers or family members, he was moved to a rehabilitation unit, with a patient-controlled analgesia (PCA) pump and catheter. Shortly after arriving, he became confused and tried to get out of bed. The nurse at the rehabilitation facility struggled during the initial assessment of this confused patient as a result of not knowing why the patient had a PCA pump and a catheter, and why he didn't have any family support.
Tips from the Joint Commission for a Better Hand-off
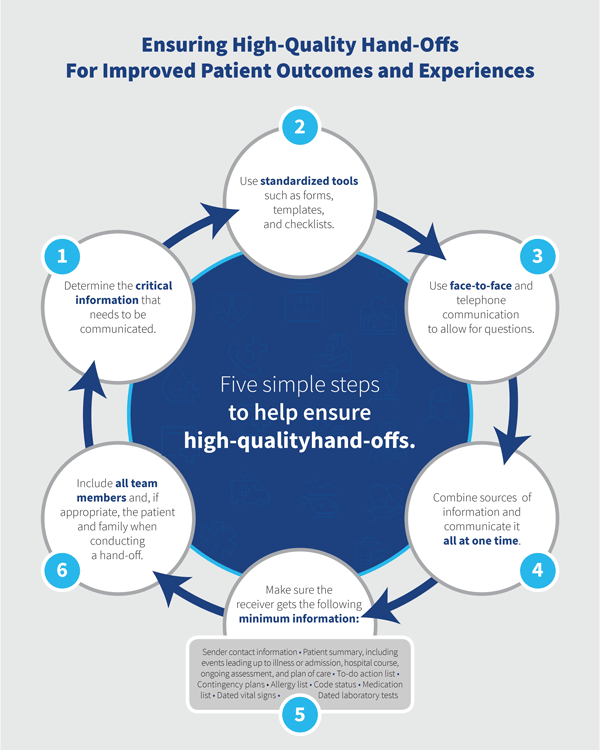
A considerable body of literature exists on improving hand-offs using a variety of methods and tools including forms and checklists as well as team training derived from evidence-based frameworks. The Joint Commission, an independent, not-for-profit organization that accredits and certifies nearly 21,000 health care organizations and programs in the United States, has provided some guidelines to ensure high-quality hand-offs.6 They include:
- Determining the critical information that needs to be communicated face-to-face and in writing, and covering everything needed to safely care for the patient in a timely fashion.
- Standardizing tools and methods used to communicate to receivers, including forms, templates, checklists, protocols, and mnemonics.
- Electronic or paper communications should not be solely relied on to hand-off the patient; face-to-face communication, telephone calls, or video conferences allow the opportunity to ask questions.
- If information is coming from many sources, combine and communicate it all at one time. Make sure the receiver gets the following minimum information: sender contact information; illness assessment, including severity; patient summary, including events leading up to illness or admission, hospital course, ongoing assessment, and plan of care; to-do action list; contingency plans; allergy list; code status; medication list; dated laboratory tests; and dated vital signs.
- When conducting hand-offs or sign-outs, do them in person in a designated location that is free from non-emergency interruptions.
- When conducting hand-offs, include all team members and, if appropriate, the patient and family, providing an opportunity to consult, discuss, and ask and answer questions.
- Electronic health records (EHRs) and other technologies, such as apps, patient portals, and telehealth, should be used to enhance hand-offs between senders and receivers, not relied upon on their own.
References
- https://www.researchgate.net/publication/49769618_Improving_Patient_Safety_Through_Provider_Communication_Strategy_Enhancements
- https://www.rmf.harvard.edu/About-CRICO/Media/In-the-News/News/2016/February/Communication-failures-linked-to-1744-deaths-in-five-years
- https://www.ucsf.edu/news/2016/03/401881/poor-communications-premature-discharges-linked-patient-readmissions-study-shows
- https://www.ncbi.nlm.nih.gov/books/NBK43663/
- https://psnet.ahrq.gov/webmm/case/134
- https://www.jointcommission.org/assets/1/18/SEA_58_Hand_off_Comms_9_6_17_FINAL_(1).pdf